About Hepatitis C Virus (HCV)
1. What is HCV ?
Hepatitis C Virus ( HCV) is the virus causing hepatitis C. Current knowledge recognizes also other viruses that cause hepatitis (e.g. HBV, HAV, HDV,HEV). The typical feature of infections caused by hepatotropic viruses is the damage to the hepatic parenchyma; however, the HCV infection - unlike the other types - in the majority of cases occurs without characteristic symptoms and may manifest itself after many years in the form of cirrhosis or hepatocellular carcinoma. According to epidemiologic studies, it is estimated that in Poland there are 200 thousand adult individuals infected with the HCV (the scope ranges from 150 to 250 thousand), which means that among 100 adult people, ~1 individual may have contact with the virus or may be infected. Unfortunately, the available data show that only one adult person out of 10 HCV-infected individuals is aware of his/her infection.
2. What is hepatitis C ?
Hepatitis C - is an infectious disease caused by the hepatitis C virus. In the early stage, which occurs between the 2nd week and the 6th month from infection, it may have a harsh course - in the form of acute hepatitis.
In the acute form, the disease symptoms may be more intense; in the majority of cases they include dyspepsia, fatigue, or - less often - jaundice. The activity of hepatic enzymes indicating the damage of the parenchyma of the liver - alanine transaminase (ALT) and asparagine aminotransferase (AST) increases several-fold than the normal upper value, not exceeding 1000 units of measure as a standard. In more cases, however, no symptoms occur at this stage of the disease. Irrespective of the course in the early phase of infection, the majority of non-treated patients develop the chronic stage of the disease, diagnosed after the relapse of 6 months from the moment of infection, in which the symptoms are moderately intensified or absent at all, and the course is very slow. In chronic infection, the activity of transaminases may increase periodically. However, in many cases there is no discernible increase in the activity of ALT and AST. However, the parenchyma of the liver becomes damaged, which may lead to cirrhosis, failure of the liver or the occurrence of the primary liver cancer.
3. What are the symptoms of the disease ?
The most frequently reported symptoms include:
- weakness
- chronic fatigue
- excessive drowsiness
- depression
- flu-like symptoms: muscular pain, pain in the joints, subfebrile states
- loss of appetite
- nausea
- vomiting
- flatulence
- reduction of body mass
- hepatic and splenic enlargement
- skin itching
- yellowing of the sclera
- skin yellowing
Unfortunately, the above-mentioned symptoms occur only in the minority of infected patients. Approximately 80% of infected individuals do not show any particular signs of the disease. Thus, disease is difficult to diagnose.
4. How can we become infected with the HCV ?
HCV is located in the blood and other tissues of the infected individual. The virus may be transmitted to other individuals directly upon the transfusion of infected blood or indirectly through commonly used objects contaminated with blood. The condition for the infection to be transmitted into another person is the damage of tissue (piercing or damageof the skin or mucous membrane), through which the virus can get inside the body of a healthy individual. Infection occurs when the virus is transmitted to the blood of the other person:
- During medical procedures connected with the damage of tissues, if no anti-infection procedures are maintained ( medical procedures that break the continuity of tissues include: injections, blood taking, dental treatment, surgeries);
- during the injection of intoxicating substances (drugs) or other agents for non-medical purposes without observing the principles of injection safety.
- during cosmetic treatments performed with the use of non-sterile sharp tools, aesthetic medicine procedures such as cosmetic pricks, piercings, tattoos, etc.);
- involving blood contact - at work or accidentally, e.g. during accidents, fight, in contact sports (e.g. boxing, judo);
- when cosmetic and hygienic tools are shared (e.g. shaving or other sharp cosmetic instruments);
A group which is particularly susceptible to blood-related infections, including the infection with HCV, are people who constantly or occasionally take drugs in the form of injections, particularly if such drugs are injected with the used equipment, or if such equipment is shared. This particularly refers to needles and syringes, but HCV may also be transmitted via other objects, e.g. pots, filters, water for drug dissolution.
Attention : the risk of infection via sexual intercourse has been evaluated as almost non-existent. However, it increases in the case of injuries and skin or mucous membrane inflammations around sex organs, anus and oral cavity. It is higher in the case of anal intercourses and practices related to the injury of mucous membranes. The transmission of the HCV is more probable with the concomitant HIV infection.
HCV may also be transmitted from the infected mother to a child during pregnancy and delivery; the risk is estimated at approximately 6% and depends on the level of viremia (amount of virus) in the mother blood, genotype of the virus and the course of the delivery. The virus is not transmitted through breastfeeding.
5. How can we detect HCV infection ?
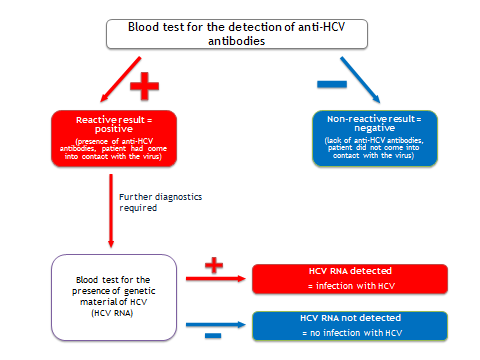
To diagnose the HCV infection, one must perform - in the first row - the blood test that is supposed to detect the presence of anti-HCV antibodies. If the result of the anti-HCV antibodies test is positive, it means that the patient has had a contact with the virus; however, a positive result of this test does not always indicate a current infection with HCV. Therefore, to confirm the infection with HCV, one should perform additional blood examination to detect the presence of a virus. Such method is, .g., a molecular test for the presence of genetic material of the HCV (HCV RNA). If the result of the molecular test is positive (namely, the blood contains the genetic material of HCV), it means that the patient is infected with the HCV virus at the time of testing.
Negative result of the HCV RNA test i.e., there is no genetic material of HCV in blood) most often indicates that the given individual is not infected with HCV, even if the presence of anti-HCV antibodies was determined in the blood before. Such result may be achieved by persons, who have experienced spontaneous elimination of HCV or who have been efficiently treated.
6. When is it recommended to make a blood test for the anti-HCV antibodies ?
A blood test for the anti-HCV antibodies is recommended in patients, who:
- have elevated blood activity of alanine transaminase enzymes (ALT) and asparagine aminotransferase (AST);
- have ever taken intravenous drugs,
- undergo chronic dialysis,
- have been born to mothers with diagnosed HCV infection,
- have had their blood transfused or their organs transplanted before July 1992,
- are hemophiliacs or were born before the year 1991,
- perform work related to the risk to infection due to professional exposure to blood-related pathogens (including doctors and nurses, medical rescuers, diagnostic laboratory technicians),
- are carriers of the HIV.
7. How can we prevent HCV infection ?
Prevention is very important!
Particular attention must be paid to observing the anti-infection procedures in medical and non-medical centers (cosmetic clinics, tattoo or beauty parlours), with particular attention on the principles of safe injections, including the use of sterile disposable tools and proper handling of multi-dose packages, keeping the aseptic rules (opening sterile equipment directly before the procedure, washing hands and using disposable gloves changed prior to each procedure, separation the area of drug preparation from the area of used equipment storage), proper sterilization of multiple-use tools, proper handling of used equipment, appropriate disinfection of surfaces which have been infected with biological material.
Quick detection and effective treatment of infected patients prevents the infection of subsequent persons and is also considered a part of preventive measures.
In the case of individuals taking drugs, the spread of HCV may be stopped by lowering the frequency of taking injected drugs, the use of sterile, disposable equipment for injections (without sharing it) and the treatment of individuals already infected. Such effects are obtained about by the broadly used damage reduction programs, encompassing the substitutive treatment of opium-based addictions, programs enhancing the availability of sterile injection equipment, education and the possibility to test individuals for infectious diseases transmitted by blood (including HCV).
Preventive measures - currently, there is no vaccine against hepatitis C. Many worldwide efforts are aiming to develop it.
8. Can the hepatitis C be treated?
Contemporary medicine makes it possible to cure the majority of cases (~70%). Treatment may be divided into symptom-oriented (e.g. decreasing the ailments) and cause-oriented, which is aimed at eliminating the virus from the body. People diagnosed with hepatitis C should consult an infectious disease specialist (through the general practitioner).
The basic purpose of the treatment is to stop or slow down the degenerative processes caused by the chronic inflammation in the liver. Treating the hepatitis C consists of the administration of antiviral drugs. Chronically HCV-infected patients are given pegylated interferon-alpha and ribavirin. For some time now, drugs acting directly on the viruses have been available (viral enzymes inhibitors, like telaprevir and boceprevir). It is a long-term treatment, lasting 16 - 72 weeks and consists of the administration of pills and an injection given on a weekly basis. Treatment is not always effective. However, constant progress of the medicine gives us the chance to use new therapeutics and new ways of treatment.